Hillrom - An AMSN Premier Partner

Getting Ahead of Patient Deterioration
Patient Safety is something we all must focus on. Hillrom and AMSN believe that no patient should die from preventable causes. We want every Med-Surg patient to be monitored for the earliest indicators of deterioration – and now, we can do that. And so can you.
With simple, secure and connected monitoring solutions that provide accurate and timely vital signs data, clinicians can make more informed decisions to enhance patient care. Real-time patient monitoring and clinical communications solutions give care teams better insights — helping to drive confident treatment decisions and proactive care.
PATIENT DETERIORATION RESOURCES
Med-Surg Moments Episode 75 - Preventing Patient Deterioration
Getting Ahead of Patient Deterioration Infographic
Early Detection and Response to Patient Deterioration in General Care Article
ESCALATING RISK FACTORS
Hospital Patients are sicker, older, and have more co-morbidities.
Nurses are spending more than 70% of their time on tasks other than direct patient care3
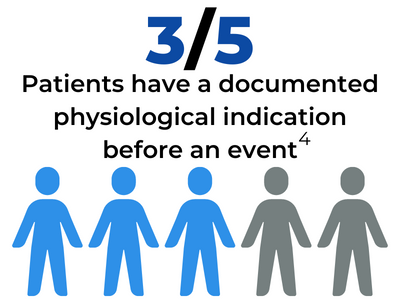
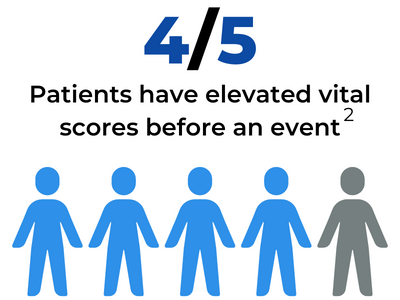
POOR OUTCOMES ARE PREDICTABLE AND PREVENTABLE
Vital sign changes can accurately predict clinical deterioration and occur several hours before a serious adverse event but often go unnoticed or are not detected until it is too late to treat.
These events include: cardiac arrest, unplanned ICU admission and/or death.
Respiratory Rates
The most accurate (and neglected) predictor of clinical deterioration5
The most common reason for unplanned ICU transfers is respiratory insufficiency or failure.6
Abnormal respiratory rates have been associated with a 13-Fold increased risk of mortality.7
Yet, respiratory rates are the most inconsistently and inaccurately recorded vital sign.
The Solution: Continuous Monitoring of Respiratory and Heart Rates
Current monitoring methods are often too little, too late, and too often wrong.
Intermittent manual monitoring of respiratory rates performed quickly by harried nurses result in frequently missed signs of early patient deterioration.
A Better Alternative in Smart Beds
Smart Beds with contact-free, continuous monitors integrated in the bed continuously monitor patients' respiratory and heart rates with proven results.
One med-surg unit that used the monitoring technology saw:8
- 86% reduction in code blue events following the implementation of Contact-Free, continuous Monitoring in a chart review study
- 45% reduction in the number of ICU days for patients transferred from Med-Surg units
- 9% reduction in Med-Surg length of stay
Continuous monitoring outcomes resources
Smart Bed Solutions for Patient Deterioration White Paper
The Problem: Patient Deterioration Infographic
Early Detection of Patient Deterioration Triggers Quick Intervention White Paper
Early Interventions for Covid-19 Patients Case Study
Nurse Assessment of Contact-Free Continuous Monitoring Technology to Identify Patient Deterioration on Inpatient Medical Surgical Units Poster
Early Detection of Patient Deterioration Using Novel Monitoring System Poster
Impact of Nursing Safety Initiatives on Patient Safety Poster
Education Resources
Practice Resources
- Med-Surg Moments Episode 80 - Improving the Nursing Burden Podcast
- The Problem: Patient Deterioration Infographic
- Smart Bed Solutions for Patient Deterioration White Paper
- Are you Detecting the Earliest Signs of Patient Deterioration? White Paper
- Early Detection of Patient Deterioration Using Novel Monitoring System Poster
- Early Detection of Patient Deterioration Triggers Quick Intervention White Paper
- Nurse Assessment of Contact-Free Continuous Monitoring Technology to Identify Patient Deterioration on Inpatient Medical Surgical Units Poster
- Impact of Nursing Safety Initiatives on Patient Safety Poster
Product Showcase
- Centrella Smart+ Bed: Contact-Free, Continuous Monitoring Presentation
- Wireless Smart+ Beds: Essential Medical Devices for Patient Safety and Connected Care White Paper
Partner Highlights
References
1. Ben-Ari, J., Zimlichman, E., Adi, N., & Sorkine, P. (2010). Contactless respiratory and heart rate monitoring: Validation of an innovative tool. J Med Eng Technol, 34(7–8), 393–398.
2. Navigant Consulting, Inc. - Analysis of Healthcare Claims data (HCUP-INS), Page 58.
3. Westbrook et al. BMC Health Services Research 2011, 11:319. http://www.biomedcentral.com/1472-6963/11/319.
4. J. Kause. Resuscitation. 2004.
5. Churpek, M. M., Adhikari, R., & Edelson, D. P. (2016). The value of vital sign trends for detecting clinical deterioration on the wards. Resuscitation, 102, 1–5. https://doi.org/10.1016/j.resuscitation.2016.02.005.
6. Bapoje SR, Gaudiani JL, Narayanan V, Albert RK, Causes of Unplanned ICU Transfers. J. Hosp. Med 2011;2;68-72. doi:10.1002/jhm.812
7. Elliott, M. (2016). Why is respiratory rate the neglected vital sign? A narrative review. International Archives of Nursing and Health Care, 2(3). https://research.monash.edu/en/publications/why-is-respiratory-rate-the…
8. Brown, H et al. the American Journal of Medicine. 2014; 127:226-232.